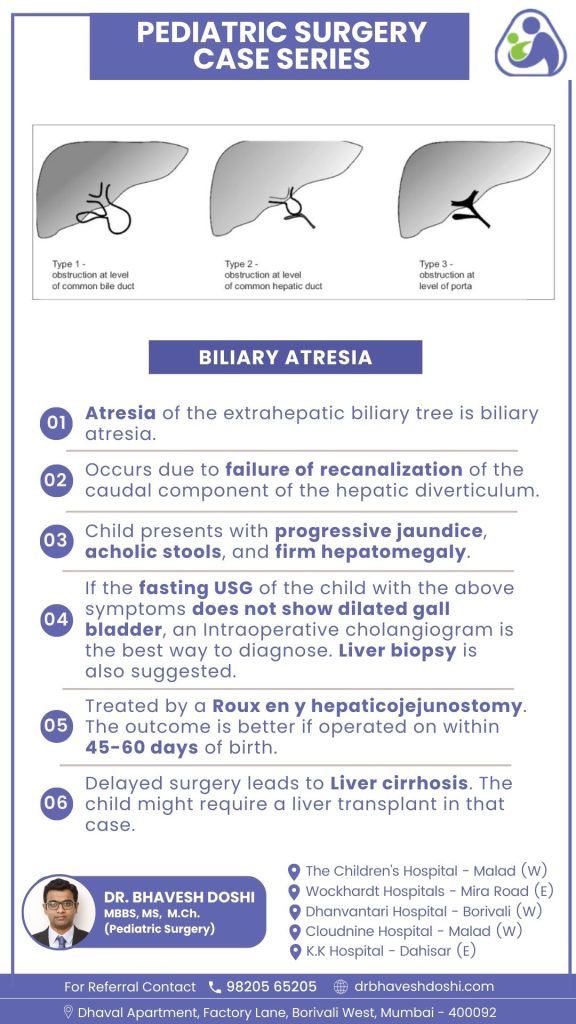
Biliary Atresia
Biliary atresia is a liver condition in babies where the tubes that carry bile are blocked.
The condition results from the incomplete development of the lower part of the hepatic diverticulum. Children with biliary atresia typically show signs such as progressive jaundice, acholic stools, and firm hepatomegaly.
How to diagnose Biliary atresia in children?
Fasting Ultrasound Assessment:
- In cases where a child presents with symptoms of biliary atresia, a fasting ultrasound is often the initial diagnostic step.
- The absence of a dilated gallbladder in the ultrasound suggests the need for further investigations.
Intraoperative Cholangiogram (IOC):
- In instances where fasting ultrasound results are inconclusive, an intraoperative cholangiogram becomes the preferred diagnostic tool.
- This procedure involves injecting contrast dye into the bile ducts during surgery, allowing for detailed X-ray imaging.
- IOC provides real-time visualization, aiding in the identification of any blockages or abnormalities in the bile ducts.
Liver Biopsy:
- A liver biopsy is recommended as a complementary diagnostic measure, offering additional insights into the liver’s condition.
- It involves the extraction of a small tissue sample from the liver for microscopic examination.
- The biopsy helps assess the extent of liver damage and contributes to a more comprehensive diagnostic evaluation.
Comprehensive Diagnostic Approach:
- The combination of intraoperative cholangiogram and liver biopsy enhances diagnostic accuracy.
- This comprehensive approach ensures a thorough assessment, especially when standard imaging alone may not provide conclusive results.
- Early and precise diagnosis is crucial for initiating timely interventions in cases of biliary atresia.
What is the treatment approach for Biliary Atresia?
Roux-en-Y Hepaticojejunostomy
Children diagnosed with biliary atresia undergo treatment through a surgical procedure known as Roux-en-Y hepaticojejunostomy. This involves creating a new connection between the liver and the small intestine, bypassing the blocked bile ducts. The Roux-en-Y technique ensures a proper flow of bile from the liver to the intestine, addressing the obstruction caused by biliary atresia.
What is the optimal timing for surgery?
The success of the treatment is notably influenced by the timing of the surgery. Operative intervention within 45-60 days of birth has shown better outcomes. Early surgical correction helps establish proper bile flow, preventing further complications associated with biliary atresia.
What are the consequences of delayed surgery?
Liver Cirrhosis and Transplantation:
Delayed surgical intervention increases the risk of developing liver cirrhosis, a condition characterized by irreversible scarring of the liver tissue. Liver cirrhosis adversely affects liver function and can lead to various complications.
In cases where surgery is significantly delayed, and liver cirrhosis has progressed, the child may require a liver transplant. Liver transplantation becomes a viable option to address the compromised liver function and improve the child’s overall health. Timely surgical intervention remains crucial in preventing the progression to advanced liver disease and the need for transplantation, highlighting the importance of early diagnosis and intervention in managing biliary atresia.



