Choledochal Cyst
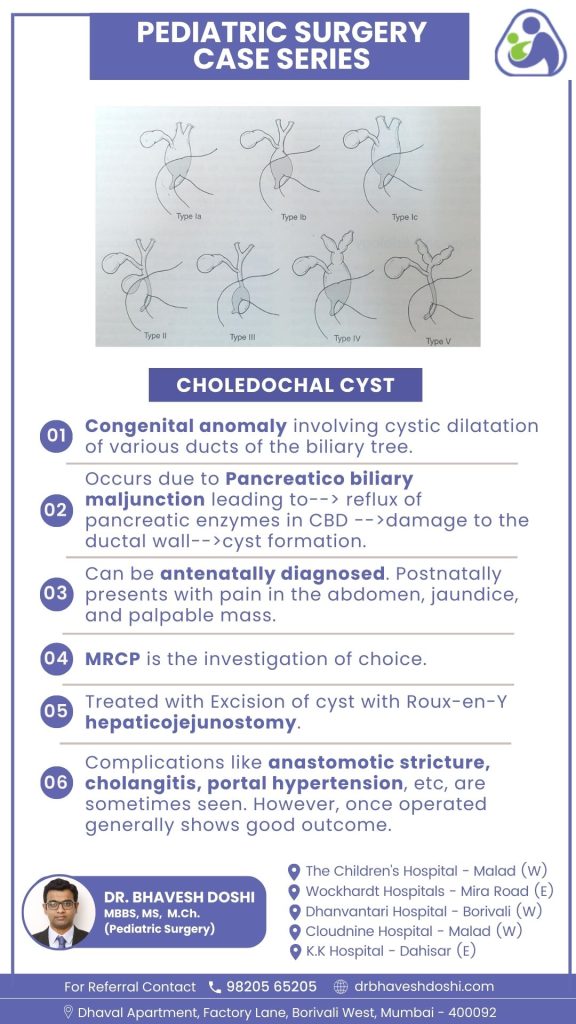
Choledochal cysts are congenital anomalies involving cystic dilatation in various ducts of the biliary tree. This anomaly arises due to pancreaticobiliary maljunction, leading to the reflux of pancreatic enzymes into the common bile duct (CBD). This reflux causes damage to the ductal wall, ultimately resulting in cyst formation.
The choledochal cyst, a rare anomaly and sometimes regarded as a premalignant condition, often presents a diagnostic challenge due to its nonspecific features. The typical manifestations include jaundice, abdominal pain, and a palpable abdominal mass. When investigating patients with these symptoms, healthcare teams must maintain a high clinical suspicion for choledochal cysts. Given the vague nature of symptoms and physical findings, accurate diagnosis relies on essential imaging studies. Excision of the choledochal cyst has demonstrated excellent outcomes, boasting an 89% event-free rate and an overall 5-year survival rate exceeding 90%. Therefore, early identification and appropriate management are imperative for optimal results and a favorable prognosis.
What symptoms are commonly observed in individuals postnatally, especially for children?
However, postnatally, individuals with this condition may present with symptoms such as abdominal pain, jaundice, and a palpable mass. The manifestation of symptoms typically occurs around the age of 5.
How are choledochal cysts diagnosed before birth?
Choledochal cysts can be identified before birth through prenatal diagnostic imaging techniques such as ultrasound.
Ultrasonography (US):
- Prenatal Diagnosis: Choledochal cysts can be identified prenatally through abdominal ultrasound as cystic structures near the porta hepatis.
- Postnatal Imaging: Ultrasonography is the initial preferred imaging modality postnatally, offering good sensitivity (71% to 97%) in identifying cysts and providing information on location and portal structures. However, it may not always reveal the cause or detect anomalous pancreaticobiliary junction (APBJ).
Computed Tomography Cholangiography (CT Cholangiography):
- CT cholangiography is more accurate than ultrasound, especially for type IV and V cysts, identifying intrahepatic duct dilation and aiding in surgical planning. Sensitivity is 90% for diagnosing choledochal cysts and 64% for characterizing the pancreatic duct.
Technetium-99 Hepatobiliary Iminodiacetic Acid Scan (Technetium-99 HIDA Scan):
- Used in neonates to differentiate between choledochal cysts and biliary atresia. Sensitivity is high (100%) for type I CCs but decreases to 67% for type IVA CCs.
Magnetic Resonance Cholangiopancreatography (MRCP):
- Gold Standard: MRCP is the gold standard for choledochal cyst diagnosis with very high sensitivity (90% to 100%). It is noninvasive, lacks ionizing radiation, and helps identify associated conditions such as APBJ, cholangiocarcinoma, and choledocholithiasis.
Endoscopic Retrograde Cholangiopancreatography (ERCP):
- Highest Diagnostic Accuracy: While ERCP offers the highest diagnostic accuracy, its invasive nature and potential complications limit its use. It is particularly beneficial for type III CCs (choledochoceles) where endoscopic sphincterotomy can be performed.
What is the treatment of Choledochal Cysts?
The primary mode of treatment for choledochal cysts involves surgical intervention. The procedure includes the complete excision of the cyst and the implementation of Roux-en-Y hepaticojejunostomy. Through excision, the cyst is entirely removed, eliminating potential complications. The Roux-en-Y hepaticojejunostomy establishes a new connection between the hepatic ducts and the jejunum, rerouting bile flow. This surgical approach aims to prevent recurrent infections, stone formation, and mitigate the risk of malignancy associated with the cyst.
What are the Complications and Postoperative Outcomes of Choledochal Cyst Surgery?
Surgical intervention for choledochal cysts generally yields positive outcomes, but complications may occasionally arise. Anastomotic stricture, cholangitis, and, in rare cases, portal hypertension are potential postoperative issues. These complications highlight the importance of vigilant postoperative management and regular follow-up to ensure optimal recovery and minimize adverse effects.
Despite these challenges, the majority of individuals who undergo surgery for choledochal cysts experience successful outcomes. Timely identification and management of complications contribute to the overall positive prognosis associated with the surgical treatment of choledochal cysts.



