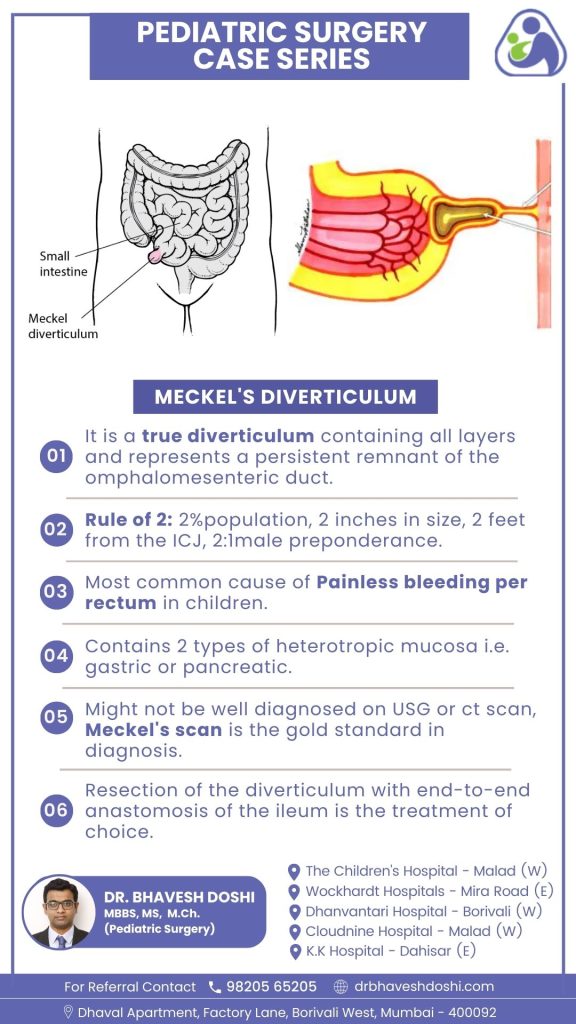
Meckel’s Diverticulum
Meckel’s diverticulum arises from the incomplete closure of the omphalomesenteric duct during embryonic development, standing as the most prevalent congenital anomaly in the gastrointestinal (GI) tract. This incomplete closure leads to the formation of a diverticulum within the small intestine. Many cases are asymptomatic. However, the presence of ectopic gastric mucosa within the diverticulum may lead to symptoms like gastrointestinal bleeding and abdominal pain.
What is “Rule of 2” in Meckel’s Diverticulum?
Meckel’s diverticulum is identified in approximately 2% of the population, making it a relatively common anatomical variation. In terms of size, this diverticulum typically measures 2 inches or less, providing a specific criterion for its dimensions. Positioned around 2 feet proximal to the ileocecal junction in the small intestine, its location is a distinctive characteristic. Additionally, there is a significant gender predisposition, with a 2:1 male preponderance, indicating that males are affected twice as often as females.
What is the most common cause of Meckel’s Diverticulum in children?
Suspect Meckel’s diverticulum in children under the age of 2 presenting with painless rectal bleeding. It constitutes around 50% of all instances of lower gastrointestinal bleeding in children within this age group
What types of heterotopic mucosa can be found in Meckel’s diverticulum?
Gastric Heterotopic Mucosa:
- Gastric mucosa within Meckel’s diverticulum means that there are cells similar to those lining the stomach. This ectopic gastric tissue can lead to acid secretion, contributing to symptoms such as abdominal pain and gastrointestinal bleeding.
Pancreatic Heterotopic Mucosa:
- The presence of pancreatic mucosa implies the existence of tissue resembling the cells in the pancreas. This heterotopic pancreatic tissue within the diverticulum can add to the diversity of cell types and functions present in Meckel’s diverticulum.
How to diagnose Meckel’s diverticulum?
Meckel Radionuclide Scan (Meckel Scan):
The most sensitive diagnostic test for Meckel’s diverticulum involves a Meckel radionuclide scan, commonly known as a Meckel scan. This nuclear study employs the injection of technetium-99m, which is absorbed by the ectopic gastric mucosa, allowing for the visualization of the Meckel diverticulum. Enhancements in dye uptake can be achieved using cimetidine or glucagon.
Contrast Extravasation in Active Bleeding:
In cases of active bleeding, a tagged Red Blood Cell (RBC) scan is employed to detect Meckel’s diverticulum. During ongoing bleeding, contrast extravasation becomes evident in the angiogram.
CT Scan for Inflammation or Obstruction:
A computed tomography (CT) scan of the abdomen and pelvis may reveal evidence of inflammation or obstruction at the Meckel diverticulum.
Invasive Methods for Diagnosis:
Mesenteric angiography is utilized to identify anomalous superior mesenteric artery branches feeding the diverticulum. Exploratory laparoscopy serves as an invasive method for diagnostic purposes.
Angiogram Indications:
Angiography is indicated when barium or nuclear scan results are negative. It is characterized by the finding of an anomalous superior mesenteric artery branch feeding the diverticulum.
Establishing Diagnosis in Uncertain Cases:
Diagnosis of a bleeding Meckel diverticulum can be established through a Meckel scan or mesenteric arteriography. Additional confirmatory methods include double-balloon enteroscopy and capsule endoscopy.
What is the treatment for Meckel diverticulum?
The primary therapeutic modality for addressing Meckel’s diverticulum involves surgical intervention, specifically the resection of the diverticulum followed by end-to-end anastomosis of the ileum. This surgical procedure aims at the complete removal of the Meckel’s diverticulum, a congenital pouch extending from the small intestine. Subsequently, the healthy segments of the ileum are skillfully connected in an end-to-end fashion. This approach stands as the treatment of choice due to its capacity to provide a definitive solution, effectively eliminating the source of complications associated with Meckel’s diverticulum.
The choice of resection with end-to-end ileal anastomosis is grounded in its ability to prevent recurrence, ensuring long-term relief from symptoms. By addressing the anomaly at its source, this surgical method minimizes the risk of complications and preserves the continuity of the bowel. Postoperatively, close monitoring is essential to identify and manage any potential complications, facilitating a smooth recovery for the patient.



