Necrotising Enterocolitis
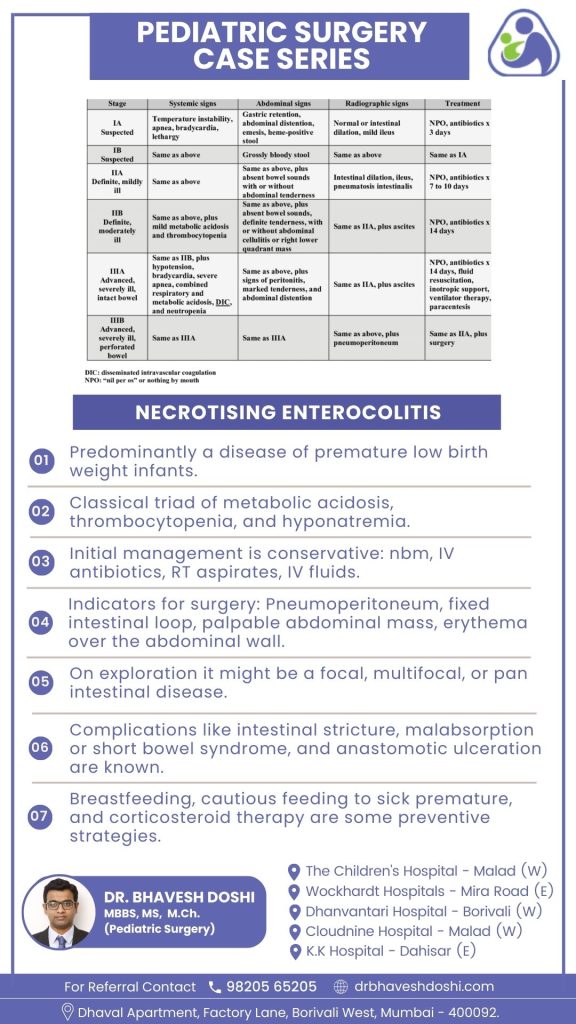
Primarily affecting premature and low birth weight infants, necrotizing enterocolitis (NEC) is a critical condition with a mortality rate reaching 50%. It presents a classic triad of metabolic acidosis, thrombocytopenia, and hyponatremia. The pathophysiology involves inflammatory processes in the intestine, leading to bacterial invasion, cellular damage, and necrosis. As NEC advances, there is a risk of intestinal perforation, resulting in peritonitis, sepsis, and potential fatality. Recognizing signs like poor feeding, vomiting, lethargy, and abdominal tenderness is crucial in the neonatal population.
How to diagnose necrotizing enterocolitis?
- The primary diagnostic tool for necrotizing enterocolitis (NEC) is an abdominal plain film series, including anterior-posterior and left lateral decubitus views.
- Diagnostic findings on the radiograph include dilated loops of the bowel, pneumatosis intestinalis, and the presence of portal venous air, which is pathognomonic for NEC.
- Pneumatosis intestinalis, the visualization of small amounts of air within the bowel wall, is characteristic of NEC, while portal venous air, though not universally present, is a poor prognostic sign when detected.
- Free air in the abdomen may indicate perforation.
- Serial abdominal radiographs, repeated every 6 hours until definitive treatment, are valuable for monitoring disease progression.
- Laboratory studies, including leukopenia with a white blood cell count below 1500 per microliter, hyponatremia, and low serum bicarbonate, are non-specific indicators.
- Blood cultures are usually negative, and a breath hydrogen test, though rarely performed, may be positive.
What is the initial approach in managing necrotizing enterocolitis (NEC)?
The initial approach involves conservative measures, such as nil by mouth (NBM), intravenous (IV) antibiotics, regular tube (RT) aspirates, and IV fluids. This allows the bowel to rest and reduces inflammation without introducing oral feedings.
What are the indications for surgical intervention in NEC?
Surgical intervention may be considered in the presence of pneumoperitoneum, fixed intestinal loop, palpable abdominal mass, and erythema over the abdominal wall. These indicators suggest complications or severe disease requiring surgical resolution.
What insights can surgical exploration provide in NEC cases?
Surgical exploration may reveal the extent of the disease, categorizing it as focal, multifocal, or pan-intestinal. Understanding the disease’s scope is crucial for planning appropriate surgical interventions and postoperative care.
What potential complications can arise post-NEC surgery?
Complications may include intestinal stricture, malabsorption or short bowel syndrome, and anastomotic ulceration. Management involves tailored nutritional support, monitoring for malabsorption signs, and prompt addressing of complications.
What preventive measures are recommended for NEC?
Preventive strategies include breastfeeding, cautious feeding for sick premature infants, and corticosteroid therapy. Breastfeeding provides essential nutrients and immune factors, cautious feeding minimizes stress on the compromised bowel, and corticosteroids may help modulate inflammation.
Prioritize infant health. Consult now to address necrotizing enterocolitis concerns with expert care. Your child’s well-being is our priority.



